Below are mostly some scientific articles on meat-related research, meta-analyses, and such; as occasionally updated. Mixed in are also some general articles discussing this area of scientific study and the implications of the evidence. A major focus is on the data that is available and lacking, but also the data that is in contradiction, specifically between Western and Asian sources. What some of the authors explain is how this is problematic in having led to unsubstantiated dietary recommendations and healthcare practices. Included further down is a section that explores a specific example, that of the so-called China Study, infamous for its low quality and faulty interpretation.
* * *
4/11/22 – As a revision, there was added new studies on meat-based diets. The most important is a recent Harvard research paper about the first carnivore diet study ever done. That has long been a criticisms, that there was no research on the carnivore diet. And it was as much, if not more, a criticism of nutrition studies than a criticism of the carnivore diet. It’s a diet that has been known about since earlier last century when an informal hospital study was done on a couple of individuals. Also, it’s long been known that some hunter-gatherer tribes follow a near-carnivore diet. So, the reluctance of research institutions and funding institutions to look into it was telling of the dominant dietary ideology, specifically as it represented contrary and inconvenient evidence. Anyway, this is a game-changer.
* * *
4/13/22 – All of this has still been on my mind, as I was noticing how much lively public debate is finally happening on these issues, after decades of suppression of public debate. It is quite refreshing. What has changed is a growing awareness of the replication crisis in nutrition studies. Researchers in the field knew about the replication crisis for a long time, but it took a while to filter out into the general public and begin to inform our critical attitude toward the older research. This was combined with improved standards for research that led to results and conclusions that challenged, contradicted, and in some cases disproved conventional wisdom, mainstream healthcare practice, and official dietary guidelines.
An example of this is the generations of fear-mongering over saturated fat. What is interesting about this is that, even though meat gets blamed, the main source of saturated fat is actually dairy. Indeed, following decades of decline of full-fat dairy, there was also a persistent takeover of plant-based fake ‘milk’. But, ironically, research shows the fake milks are worse than the real thing, for children most of all (Jen Christensen, Most young children shouldn’t drink plant-based milk, new health guidelines say). It is measurable in decreased height among children who partly or entirely drink plant milks, since they are getting less essential nutrients like calcium, vitamin D, and protein (not to mention plant proteins being less bioavailable).
There is a vast diversity of other essential and conditionally essential nutrients in dairy and other animal foods. The fat-soluble vitamins like vitamin D are particularly key, as they are hormones, hormone precursors, and hormone activators; including in determining how other nutrients (e.g., calcium) are used and where they are directed. Of course, fat-soluble vitamins are concentrated in the fat, and that fat can also have benefits. Dairy fat, much of it saturated, has been shown to prevent diabetes over the lifetime, but importantly proven effective in protecting children and adults from becoming overweight.
The mechanisms for this aren’t yet entirely known. Some suspect that the satiating effect of dairy fat, probably like any animal fat, will cause one to eat fewer carbohydrates and other calories. Indeed, there is evidence that when people imbibe low-fat dairy they compensate by increasing their carb intake. And carbs are much easier to overeat. But it’s also possible there is some molecule that upregulates fat utilization and metabolism. That is intriguing. Such dietary fats ensure the body doesn’t produce excess body fat. So, get more animal fat to stay trim! Drink the cow’s milk and eat the cow’s meat. That is the secret to a long, happy, and healthy life.
It’s not clear why animal fats got such a bad reputation. Lard has about the same ratio of monounsaturated fat (MUFAs) as olive oil, specifically oleic acid; and it is precisely because of oleic acid that olive oil is said to be so healthy. Red meat also has some MUFAs in them, if a relatively lesser percentage, but nonetheless ground beef has more MUFAs than saturated fat. Interestingly, dark chocolate has a balanced ratio of oleic acid and saturated fat stearic acid, the latter common in ruminant meat (tallow is also a concentrated source of the highly sought after conjugated linoleic acid or CLA that, like stearic acid, promotes a lean body). The major blame always goes to saturated fat, despite its intake not having increased, contrary to conventional claims; and dairy is a greater source than red meat — by the way, a new essential fat (EFA) was discovered (C15:0, pentadecylic acid, pentadecanoic acid, Fatty15, or FA15) that is most abundant in dairy fat and also higher in meat that is pasture-raised or wild-caught. Heck, coconut oil has more saturated fat than beef. Also, coconut oil and palm kernel oil are a significant source of a specific saturated fat called medium chain triglycerides (MCTs), along with dairy (particularly from goats (30-35%), sheep (10-25%), and cows (10-20%); not to mention in human breast milk (2-10%).
MCTs, although non-essential for adults, have proven to have immense benefit for energy metabolism (thermogenesis and fat oxidation) in the body in general and particularly in the brain. Combined with MCTs’ action as an appetite suppression, this might be the magical substance that limits weight gain with full fat dairy intake. They’ve gained public interest because they are the main ingredient in Bulletproof coffee, basically the one-two punch of MCTs plus caffeine (where the latter assists in fat burning). MCTs have also gained much fame in their benefiting serious neurocognitive issues such as Alzheimer’s where, because of insulin resistance in the brain, the neurons lose the capacity to use glucose and so MCTs offer an alternative source of fuel.
This is getting away from the issue of meat and even necessarily animal foods, as plant-based MCTs are popular these days; but let’s dig a bit more into these awesome saturated fats. One thing MCTs are known to do is help the body to produce ketones, even with moderate carb intake, despite ketones typically only produced at high levels (i.e., ketosis) with a consistently and strictly very low-carb diet (the kind of diet that is much easier and more satisfying to do with animal foods and animal fat). The thing is, even when carb levels are high enough to guarantee non-ketosis, MCTs still show neurocognitive benefit in studies demonstrating other pathways of action. It turns out the MCTs themselves can be used by the brain.
A related phenomenon is seen in general during early human life. From fetus to at least early teen years, it appears that all humans are continuously in a state of ketosis, according to various studies and the work of Angela A. Stanton. This might make sense for infants with their diet of MCTs from breast milk that, by the way, is loaded with sugar. Yet even older children on a high-carb diet remain in ketosis. That indicates ketones and ketosis is central to early development. Interestingly, even as all young people are presumably in ketosis, a keto diet (often including MCTs) has still benefited children with neurocognitive disorders (e.g., epileptic seizures) and serious diseases (e.g., type II diabetes).
Anyway, considering the neurocognitive advantages of MCTs, maybe it’s significant that the rise of the challenging complexities within civilization coincided with the widespread increased adult consumption of MCT-filled milk, butter, and other dairy foods. Genghis Khan and his Mongol army nearly conquered all of Eurasia on a diet consisting mostly of red meat, dairy, and blood — saturated fat galore! From butter and ghee to lard and tallow, animal fats have often been a way for farming communities, from feudal villages to pre-war Okinawa, to get an extremely concentrated source of calories and nutrients, sometimes MCTs as well, while on an otherwise limited agricultural diet.
That isn’t even to cover the hundreds of other fatty acids, saturated and otherwise, found in meat and other animal foods. A saturated fat already mentioned, the long chain stearic acid (SA), also helps the body burn fat as do MCTs. Some long chain saturated fats are odd-chained and, as has been argued, among them might be those that are essential. This is the problem as the components of animal foods have been understudied. It’s related to the problem of all the plant foods and plant-based supplements that research shows as beneficial, but when one looks deeper the same benefits often can be obtained through animal foods, a low-carb diet, fasting, exercise, etc.
Palmitic acid, palmitoleic acid, (Omega-7) mearic acid, conjugated linoleic acid (trans fat). Or consider butyrate, a short chain fatty acid (SFCA). It’s why there are official recommendations for a high-fiber diet because fermentation creates butyrate and other SFCAs. Yet butyrate is also found in dairy fat, if only at 4%. Then again, butyrate can form as well from the fermentation of animal connective tissues and collagen. Besides, on a low-carb diet, the body produces a similar molecule, beta-hydroxybutyrate. So, another plant-based talking point is shot down.
Then there is arachidonic acid (ARA) that, though an omega-6, is not inflammatory like the omega-6s in seed oils; and instead it actually regulates inflammation. It does compete for absorption and utilization with the omega-3 docosahexaenoic acid (DHA) that is more well known as an anti-inflammatory, but that probably just means the body doesn’t need both ARA and DHA in high amounts at the same time since they both have this same overlapping purpose. There might be a reason some animal foods are higher in ARA and lower in DHA (beef), while others are the reverse (cold water fatty fish). Then again, any pasture-raised or wild-caught animal food will be higher in these kinds of healthy fats.
* * *
8/15/22 – One could add much more info about the affect of meat and animal-based nutrition on mental health. The more one looks for the scientific evidence the more one finds. Of course, studies are mixed and this is a field in the middle of a replication crisis. There are more badly designed than well designed studies, unfortunately. Nonetheless, there is growing evidence, as research improves, showing the importance of animal foods. The further evidence will be included below. But let us note two basic points. Much of the evidence indicates that an animal-based diet, particularly one including meat, is strongly associated to greater mental health; specifically lower rates of mood disorders. This is unsurprising as many animal-based nutrients, from carnitine and DHA to choline and B vitamins, have been specifically studied in their positive affect on neurocognitive functioning.
A basic nutrient many people, other than weightlifters, don’t know about is creatine that, besides promoting muscle-building, is necessary for brain health and can be used to treat psychiatric disorders (Patricia J. Allen, Creatine metabolism and psychiatric disorders: Does creatine supplementation have therapeutic value?). Another interesting example, the abovementioned EFA C15:0 has anti-anxiety effects (Eric Venn-Watson, A New Take on Comfort Food: Getting the Anxiety-Lowering Effects of Food without the Calories). Depression has often been studied in terms of animal fats, specifically those high in wild-caught fish (docosahexaenoic acid or DHA) and pasture-raised ruminants (conjugated linoleic acid or CLA) (Luisa Cigliano et al, Dietary Supplementation with Fish Oil or Conjugated Linoleic Acid Relieves Depression Markers in Mice by Modulation of the Nrf2 Pathway). One could go on and on with the immense research on various animal-based nutrients. Unsurprisingly, those on extreme plant-based diets show improvements with supplementation.
Interestingly, the comparison of animal-based and plant-based diets aside, at least one study showed no difference on mental health for those eating meat versus fish (Mary Hysing et al, Fatty Fish Intake and the Effect on Mental Health and Sleep in Preschool Children in FINS-KIDS, a Randomized Controlled Trial). It could be noted, though, that meat intake was neutral for dementia, whereas fish intake lowered risk (Pascale Barberger-Gateau et al, Fish, meat, and risk of dementia: cohort study); but this could merely be increased omega-3s intake balancing out the harm of excessive omega-6s from seed oils; and so possibly there would be no difference between meat and fish if that confounder was controlled for. Almost any kind of animal flesh will apparently be beneficial, if there might be some variance depending on specific nutritional profiles; with the possible exclusion of processed meats, as some research indicates, that contain a lot of non-animal additives, although the ingredients of processed meats vary greatly and studies of them are confounded with the unhealthy user effect.
Here is a takeaway point. It’s not only what benefit might be gained from animal-based nutrition but what harm might be caused by non-animal substances that either are added to agricultural goods (e.g., glyphosate) and processed foods (preservatives, artificial flavorings, etc), including processed meats, or that are naturally found in plant foods (antinutrients like lectins, oxalates, salicylates, goitrogens, phytoestrogens, phytates, and tannins; proteins such as gliadin/gluten and zein; hormone mimics in soy; etc). Avoiding plant foods, for many people, can be as important as adding animal foods. This is what so many have found when they’ve eliminated certain plant foods or gone strict carnivore. Disabling and sometimes deadly conditions, from cancer to autoimmune disorders, have been reversed and possibly cured; but we aren’t allowed to call them cured because these diets are considered medical treatments and not normal eating patterns consistent with millions of years of hominid evolution.
Beyond that, surely eggs and dairy would have some benefits as well (Aurora Perez-Cornago, Intake of High-Fat Yogurt, but Not of Low-Fat Yogurt or Prebiotics, Is Related to Lower Risk of Depression in Women of the SUN Cohort Study; Chen Du, Relationships between Dairy and Calcium Intake and Mental Health Measures of Higher Education Students in the United States: Outcomes from Moderation Analyses; Ester Solberg, The Effects of Powdered Fertilized Eggs on Depression; etc). But that isn’t our focus here; if it is important to note that animal foods are what distinguish lacto-ovo-vegetarianism from strict plant-exclusive veganism.
There is a helpful angle to take. In one study, even as the conclusion was questionable, the data was telling (Christopher J. Hopwood, The link between vegetarian diet and depression might be explained by depression among meat-reducers). The author found that depression was more associated with meat-reduction than with vegetarianism/veganism. This might seem strange, if one is unfamiliar with other data. When asked, most vegetarians admit to eating meat and fish while vegans admit to eating animal foods; not to mention many vegetarians getting much nutrition from dairy and eggs. In knowing many vegetarians and vegans over a lifetime, we have observed that most do eat significant amount of animal foods. As a case in point, we know a self-identified vegan who regularly eats fish and daily puts cream into her coffee. Many such people are more focused on eating a plant-based diet than in eliminating animal foods. This could be why there is a major distinction between meat-reducers and vegetarians/vegans, the two not necessarily being the same.
Consider the most vegetarian population on the planet, a population that once commonly sacrificed animals to their gods, a historically recent result of the meat and fish taxes enforced by the British Empire (Rohini Krishnamurthy, ‘Indian vegetarians do not eat vegetables’). In India, 39% identify as vegetarian (almost 4 in 10, about 400 million), “according to a new Pew Research Center survey. (While there are many ways to define “vegetarian” in India, the survey left the definition up to the respondent” (Manolo Corichi, Eight-in-ten Indians limit meat in their diets, and four-in-ten consider themselves vegetarian); although multiple Indian states have +98% non-vegetarians. Overall, 81% claim to reduce meat intake, but 70% still regularly eat dairy, eggs, and fish; and “42.8% Indian women and 48.9% of men consumed poultry and meat weekly” with “barely 6% of the population eats meat on a daily basis, and nearly 40% on a weekly basis,” however ‘meat’ is being defined.
Then again, there is a problem of underreporting where, in India, eating beef is socially condemned and beef bans are sometimes enforced. Nonetheless: “A reported 7% of the population eats beef. However, this figure is disputed by many researchers, who claim that the actual statistic is closer to 15% with people unwilling to admit to eating meat due to cultural and religious factors” (Roshni Ramesan, India Has 70%+ Non-Vegetarian Population But Is Considered Vegetarian; Why?). There was no data found on how many Indian vegetarians eat ‘meat’, what kind, how often, and under what circumstances. We can’t assume that vegetarianism always means never eating meat or even not eating meat regularly, and that goes doubly in speaking about other cultures. The main reason people all over the world eat less meat than they otherwise would is simply the costs of meat and the commonality of poverty. The main point is most people across all countries, maybe including most vegetarians, eat meat when it’s available.
Plus, based on an old cultural bias going back to the ancient world, many vegetarians and vegans don’t consider fish to be meat and others are also willing to make an exception for chicken. Combined with dairy and eggs, that can potentially be enough animal-based nutrition to avoid the worst deficiency-related health conditions and diseases. Anyway, most people on such diets aren’t doing so for dogmatic principles: “the majority (54%) of vegetarians were open to the possibility of eating meat. […] Despite the fact that eating meat fundamentally defies the definition of being a vegetarian, meat-eating vegetarians appear to comprise a substantial proportion of the vegetarian population: For example, a study by Kwan and Roth (2004) revealed that 40% of self-identified vegetarians actually eat meat” (Daniel L. Rosenfeld, What Does It Take to Get a Vegetarian to Eat Meat? Factors Predicting Dietary Adherence).
Other data shows it to be a much higher number: “A poll conducted by CNN surveyed 10,000 Americans about their eating habits, and roughly 6% of the respondents self-identified as vegetarians. The researchers then asked individuals to describe their eating habits, and 60% of the “vegetarians” reported having eaten meat within the last 24 hours. Okay, that could’ve have been a fluke (or just a really, really dumb sample group). Then the U.S. Department of Agriculture conducted a similar study. This time, they telephoned approximately 13,000 Americans, and 3% claimed to be vegetarians. When they followed up a week later, 66% of the self-proclaimed veggie-lovers had eaten meat the day before” (Erika Grant, SURVEY: 60% Of Self-Proclaimed Vegetarians Ate Meat Yesterday). If two-thirds of vegetarians eat meat on a daily basis, then what kind of ‘vegetarianism’ are we talking about. Talk about a confounding factor. This calls into question every scientific study and survey ever done in studying ‘vegetarianism’, specifically in comparing ‘vegetarianism’ with meat-inclusive diets.
There are many reasons meat-abstainers lapse, a common reason being drunkenness, but even without alcohol many regularly imbibe animal flesh: “34% said every time they drink, 26% said fairly often, 22% said rarely, and 18% said occasionally” (Mary Bowerman, Survey: 1 in 3 vegetarians admits to eating meat when drunk). For a significant number, they might not perceive it as a lapse at all: “Some vegetarians reported that they view their diets as flexible guidelines, rather than rigid rules they ought to follow without exception” (Daniel L.Rosenfeld & A. Janet Tomiyama, When vegetarians eat meat: Why vegetarians violate their diets and how they feel about doing so). Many vegans in particular and many vegetarians as well openly admit that their ideological position is not primarily about diet but more broadly about an ethical lifestyle, which is why any diet that adheres to the least harm principle can be reasonably and fairly labeled as ‘vegan’ (Carnivore Is Vegan).
Even then, most of these supposed plant-based meat-abstainers or merely meat-reducers go back to regularly eating meat (Faunalytics, A Summary Of Faunalytics’ Study Of Current And Former Vegetarians And Vegans). Most vegetarians and vegans couldn’t even last a year on the diet, a third not making it beyond three months, and most of the rest giving up within a few years (Colin Schultz, Most Vegetarians Lapse After Only a Year), “with 9 years being the average length of time of abstinence” (Sarah Pope, Most Vegetarians Return to Eating Meat due to Failing Health) and the average age being quite young at 28 years old, which means most of them spent their first couple of decades or so eating meat (Scritto da Redazione, Why do most vegetarians go back to eating meat?); such that “ex-vegetarians outnumber current vegetarians by a ratio of three to one, suggesting that 75% of vegetarians lapse” (Guy McCardle, Lapsed Vegetarians or, Return of the Meat-Eaters). The main reason given for ending their meatless experiment was declining health and persistent physical weakness, while others noted animal-based cravings and a general sense of constant hunger. Hunger for meat is built into our biology from evolution. For optimal health, we need animal-based nutrition and, no matter our personal ideology, our bodies know what we need.
Plant-based advocates can’t deny the failure of this ideological project — more from Sarah Pope: “Even the 2017 Netflix documentary What The Health was unable to name a single vegan population group that was successful long term! […] I submit that the results of this survey are not surprising and are in fact a testament to the research of Dr. Weston A. Price. Dr. Price traveled the world in the 1920s and 1930s visiting 14 isolated cultures in the process. During this adventure which he documented in great detail with amazing pictures in his masterpiece Nutrition and Physical Degeneration, Dr. Price concluded that while the diets of these natives varied widely, nutrient dense animal foods high in the fat soluble vitamin A, D, and K2 (also known as Activator X) were the common denominator. Consumption of these animal foods were revered in these communities as they bestowed vibrant health, easy fertility, healthy children, and high resistance to chronic and infectious disease.
“This discovery was a disappointment to Dr. Price who had expected to find the vegetarian cultures to be the healthiest cultures of all. But, the vegetarian cultures he examined displayed far more degeneration and tooth decay than the omnivore cultures. This surprised him given that these vegetarian cultures did indeed have superior health than the Americans of his day. However, he could not deny that the health of the indigenous omnivores exceeded that of the vegetarian cultures. Those consuming a wide variety of marine seafoods exhibited the most vibrancy of all.” One of Dr. Price’s expectations actually was of discovering a plant-exclusive traditional community, somewhere in the world, but he never did find such a mythical creature. Knowing what we now know, this is the opposite of surprising. By the way, as related to mental health, Dr. Price observed populations that had plentiful fatty animal foods (i.e., nutrient-density) in their diet exhibited greater ‘moral health’: happier, friendlier, kinder, and more helpful.
* * *
A major health organization says meat, eggs and milk are vital sources of ‘much-needed nutrients.’ Here’s why
by L’Oreal Thompson Payton
A new report from the United Nations’ Food and Agriculture Organization (FAO) has determined that meat, eggs and milk are vital sources of much-needed nutrients, such as proteins, fats and carbohydrates, that aren’t easily found in plant-based foods.
The comprehensive study, which is based on data from more than 500 scientific papers and 240 policy documents, also stated that these nutrients are critical during key life stages, such as pregnancy and lactation, childhood, adolescence and older age.
Nina Teicholz Tweeted:
Meat cannot be causing diabetes, obesity, kidney disease etc.
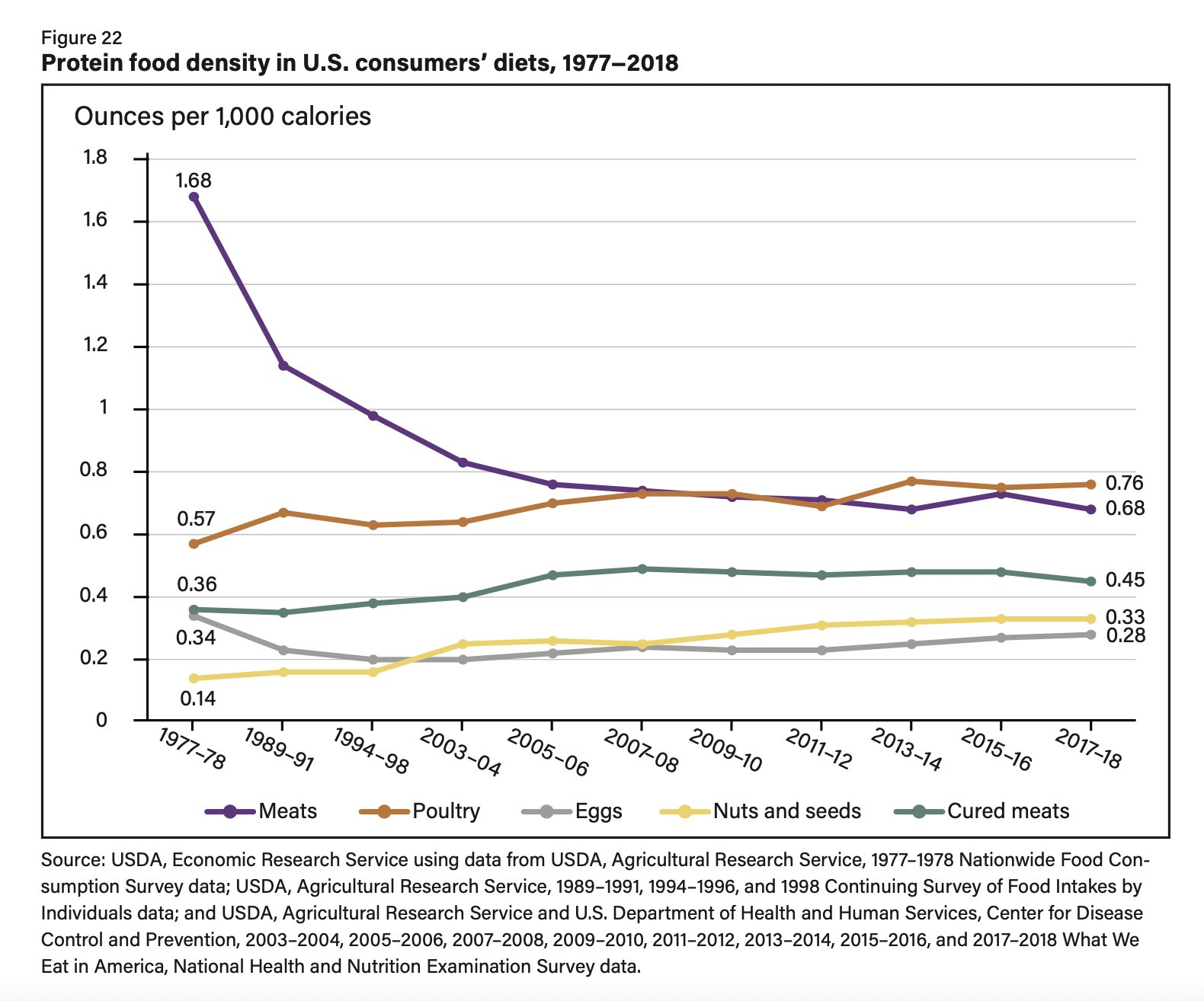
Here’s USDA data from 1977-2018.
Disease rates have skyrocketed during these years, yet meat consumption (the purple line) declined–a lot. Stop vilifying meat–it’s not the problem.
Tweet Responses
A Big Mac combo, regular size with coke, has the following macros:
– 1060 calories
– 128 g carbs
– 49 g fat
– 30 g protein
But the anti-meat folks say that meat is what is making people unhealthy.
McDonald’s Nutrition Calculator
60% of the American diet is grains, added sugars, and vegetable oils but I’m sure it’s the 16% of calories from meat that are causing the issues.
[In fact, 77% of the standard American Diet (SAD) is plant foods. While intake of beef and saturated fat has been declining for decades, with fewer heads of cattle than in the 1980s. ~BDS]
Dietary Quality by Food Source and Demographics in the United States, 1977-2018
by by Bing-Hwan Lin, Joanne Guthrie, & Travis Smith
31 Studies Disproving Veganism (video)
by Joey A. Schwartz
Study linking deaths to red meat ‘appears implausible’ and ‘lacks transparency’
by Flora Southey
Do Vegetarian Diets Provide Adequate Nutrient Intake during Complementary Feeding? A Systematic Review
by Giovanni Simeone, et al
For ethical reasons, there are no interventional studies assessing the impact of non-supplemented vegetarian/vegan diets on the physical and neurocognitive development of children, but there are numerous studies that have analyzed the effects of dietary deficiencies on individual nutrients. Based on current evidence, vegetarian and vegan diets during the complementary feeding period have not been shown to be safe, and the current best evidence suggests that the risk of critical micronutrient deficiencies or insufficiencies and growth retardation is high: they may result in significantly different outcomes in neuropsychological development and growth when compared with a healthy omnivorous diet such as the Mediterranean Diet. There are also no data documenting the protective effect of vegetarian or vegan diets against communicable diseases in children aged 6 months to 2–3 years.
Debunking the vegan myth: The case for a plant-forward omnivorous whole-foods diet
by James H O’Keefe, Evan L O’Keefe, Carl J Lavie, & Loren Cordain
Vegan diets are widely promoted as protective against cardiovascular disease (CVD); however, removing all animal foods from a human’s diet usually causes unfavorable health consequences. Our hominin ancestors began consuming meat, fish, seafood, and eggs >2 million years ago. Consequently, humans are genetically adapted to procure nutrients from both plant and animal sources. In contrast, veganism is without evolutionary precedent in Homo sapiens species. Strict adherence to a vegan diet causes predictable deficiencies in nutrients including vitamins B12, B2, D, niacin, iron, iodine, zinc, high-quality proteins, omega-3, and calcium. Prolonged strict veganism increases risk for bone fractures, sarcopenia, anemia, and depression. A more logical diet is a plant-forward omnivorous eating pattern that emphasizes generous consumption of natural, unprocessed foods predominantly from plants. To balance this diet, modest amounts of wholesome animal foods, such wild-caught fish/seafood, pasture-raised meat and eggs, and fermented unsweetened dairy should be consumed regularly.
Meat and mental health: a systematic review of meat abstention and depression, anxiety, and related phenomena
by Urska Dobersek, Gabrielle Wy, Joshua Adkins, Sydney Altmeyer, Kaitlin Krout, Carl J. Lavie, & Edward Archer
Studies examining the relation between the consumption or avoidance of meat and psychological health varied substantially in methodologic rigor, validity of interpretation, and confidence in results. The majority of studies, and especially the higher quality studies, showed that those who avoided meat consumption had significantly higher rates or risk of depression, anxiety, and/or self-harm behaviors. There was mixed evidence for temporal relations, but study designs and a lack of rigor precluded inferences of causal relations. Our study does not support meat avoidance as a strategy to benefit psychological health.
Red meat consumption and mood anxiety disorders
by Felice N. Jacka, Julie A. Pasco, Lana J. Williams, Neil Mann, Allison Hodge, Laima Brazionis, & Michael Berk
The fact that red meat was a prominent component of this protective dietary pattern was of some interest, as previous studies examining dietary patterns as predictors of illness have observed red meat to be a part of unhealthy dietary patterns (e.g. [9-11]). Moreover, there are published studies from Australia [12] and Scandinavia [13] reporting that vegetarians and/or low meat consumers have poorer mental health than those who habitually eat meat, although the direction of the relationship between vegetarian status and mental health is unclear. […]
For those women consuming less than the recommended intake of red meat per week, the odds for MDD/dysthymia were more than doubled compared to those consuming the recommended intakes. Similarly, those women with low red meat consumption were nearly twice as likely to have an anxiety disorder. Adjusting for ‘traditional’ dietary patern scores resulted in strengthening of the relationship between high meat intake and these variables (table 1).
Meat Consumption Associated with Less Anxiety and Depression
by Joseph E. Scherger
Twenty studies met the selection criteria, representing 171,802 participants (157,778 meat consumers and 13,259 meat abstainers). Most studies showed meat abstainers recorded higher rates of depression, anxiety, and self-harm, including suicide. Meat abstainers also were more likely to be prescribed medication for mental health problems. Conversely, the authors observed meat consumption was associated with significantly lower rates of depression ( P < 0.001) and anxiety ( P = 0.02). Their analysis showed the more rigorous the study, the more positive and consistent the relation between meat consumption and better mental health.
Evolutionary biologists have shown ancient Homo sapiens were omnivores who ate both animal and plant foods. 1,2 Our relatively large brains and narrow waistlines reflect this. […] People who were vegans for many years have reported a dramatic improvement in their well-being once they varied their diet to include healthy animal products.
Meat and mental health: A meta-analysis of meat consumption, depression, and anxiety
by Urska Dobersek, et al
In this meta-analysis, we examined the quantitative relation between meat consumption or avoidance, depression, and anxiety. In June 2020, we searched five online databases for primary studies examining differences in depression and anxiety between meat abstainers and meat consumers that offered a clear (dichotomous) distinction between these groups. Twenty studies met the selection criteria representing 171,802 participants with 157,778 meat consumers and 13,259 meat abstainers. We calculated the magnitude of the effect between meat consumers and meat abstainers with bias correction (Hedges’s g effect size) where higher and positive scores reflect better outcomes for meat consumers. Meat consumption was associated with lower depression (Hedges’s g = 0.216, 95% CI [0.14 to 0.30], p < .001) and lower anxiety (g = 0.17, 95% CI [0.03 to 0.31], p = .02) compared to meat abstention. Compared to vegans, meat consumers experienced both lower depression (g = 0.26, 95% CI [0.01 to 0.51], p = .041) and anxiety (g = 0.15, 95% CI [-0.40 to 0.69], p = .598). Sex did not modify these relations. Study quality explained 58% and 76% of between-studies heterogeneity in depression and anxiety, respectively. The analysis also showed that the more rigorous the study, the more positive and consistent the relation between meat consumption and better mental health. The current body of evidence precludes causal and temporal inferences.
Higher Non-processed Red Meat Consumption Is Associated With a Reduced Risk of Central Nervous System Demyelination
by Lucinda J. Black, et al
The evidence associating red meat consumption and risk of multiple sclerosis is inconclusive. We tested associations between red meat consumption and risk of a first clinical diagnosis of central nervous system demyelination (FCD), often presaging a diagnosis of multiple sclerosis. We used food frequency questionnaire data from the 2003–2006 Ausimmune Study, an incident, matched, case-control study examining environmental risk factors for FCD. We calculated non-processed and processed red meat density (g/1,000 kcal/day). Conditional logistic regression models (with participants matched on age, sex, and study region) were used to estimate odds ratios (ORs), 95% confidence intervals (95% CI) and p-values for associations between non-processed (n = 689, 250 cases, 439 controls) and processed (n = 683, 248 cases, 435 controls) red meat density and risk of FCD. Models were adjusted for history of infectious mononucleosis, serum 25-hydroxyvitamin D concentrations, smoking, race, education, body mass index and dietary misreporting. A one standard deviation increase in non-processed red meat density (22 g/1,000 kcal/day) was associated with a 19% reduced risk of FCD (AOR = 0.81; 95%CI 0.68, 0.97; p = 0.02). When stratified by sex, higher non-processed red meat density (per 22 g/1,000 kcal/day) was associated with a 26% reduced risk of FCD in females (n = 519; AOR = 0.74; 95%CI 0.60, 0.92; p = 0.01). There was no statistically significant association between non-processed red meat density and risk of FCD in males (n = 170). We found no statistically significant association between processed red meat density and risk of FCD. Further investigation is warranted to understand the important components of a diet that includes non-processed red meat for lower FCD risk.
The case for red meat
by George Henderson
Several observational studies have looked at the characteristics of meat-avoiding populations and found alarming increases in depression, anxiety and self-harm.
“The majority of studies, and especially the higher quality studies, showed that those who avoided meat consumption had significantly higher rates or risk of depression, anxiety, and/or self-harm behaviors. There was mixed evidence for temporal relations, but study designs and a lack of rigor precluded inferences of causal relations. Our study does not support meat avoidance as a strategy to benefit psychological health.”[3]
How can we explain these correlations? Why should we assume that they are causal?There are several lines of evidence to support a causal link:
1) several nutrients found in meat and animal foods are important factors in mood and cognition; vitamin B12, iron, carnitine, DHA, choline and tryptophan are some examples.[4]
2) the fatty acid mix in dairy and red meat has a similar composition to that of amniotic fluid and breast milk which has anxiolytic (anti-anxiety) effects in young animals.[5]
3) soy is a convenient and cheap replacement for animal protein; soy processing in Western diets results in a 10-fold higher level of the estrogenic contaminant isoflavone than that found in Asian diets.[6] Soy isoflavone causes anxiety behaviour in young female animals, and there is evidence supporting psychotropic and hormonal effects in humans.[7,8,9.10] Interestingly, while right-wing critiques of soy eating focus on effects it can have on young men, the scientific evidence for adverse effects in younger females, converting to HRT-like benefits after menopause, is stronger.[11]
4) other toxins found in plants, such as salicylates and oxalates, as well as problematic proteins such as gliadin/gluten and zein, may be present at higher levels in meat-free diets (but are not unique to them). A vegan mince sold in Countdown supermarkets is simply a coloured blend of soy protein and gluten, a protein linked to the risk of schizophrenia.[12]
In the New Zealand context it would be relatively easy to confirm or dispute some of these associations. Everyone admitted to hospital for longer than a day supplies their dietary preferences. The dietetic preference data from psychiatric admissions could be both linked to outcomes over time and compared with the population average distribution, or the distribution in a ward where diet is least likely to play a role in admissions.
Dietary Recommendations for Familial Hypercholesterolaemia: an Evidence-Free Zone
by David M Diamond, et al
Key points
- Current dietary guidelines for management of coronary heart disease (CHD) risk in familial hypercholesterolaemia (FH) are based on the diet-heart hypothesis, which is outdated and unsupported.
- There is no evidence to support the recommendation that FH individuals should consume a low saturated fat, low cholesterol diet.
- A low carbohydrate diet (LCD) significantly improves cardiovascular disease biomarkers, compared with a low fat diet.
- There is sufficient rationale for conducting clinical trials to assess the effects of an LCD on FH individuals with an insulin-resistant phenotype.
- Extensive research has documented that hypercoagulation is a more important risk factor for CHD than low-density lipoprotein cholesterol in FH. Therefore, LCD trials should include FH subjects with an elevated risk of hypercoagulation.
Consumption of Unprocessed Red Meat Is Not a Risk to Health
from World Farmers’ Organisation (WFO) Scientific Council
A synopsis of five significant, recent and broad-scale scientific investigations on the health risks and health benefits of red meat consumption indicates that there is no convincing scientific evidence for assertions about harmful health effects of unprocessed red meat intake. If at all, the data very slightly lean toward an association of red meat consumption and protective health benefits. Overall, any of the statistical associations of up to 100 grams of red meat consumption per capita per day are so weak that they should be considered neutral. It is notable that less than 1% of the global population consumes more than 85 grams of red meat per day. From a global public health perspective, then, red meat consumption above the threshold of 85 grams is so negligible as to be irrelevant. National governments and supranational organizations such as the EU and UN, and their initiatives such as this year’s UN Food Systems Summit, as well as international business and consumer associations, would be wrong to assume that a scientific consensus exists to justify policies to reduce red meat consumption in the general population for health reasons.
Associations of unprocessed and processed meat intake with mortality and cardiovascular disease in 21 countries [Prospective Urban Rural Epidemiology (PURE) Study]: a prospective cohort study
by Romaina Iqbal, et al
In a large multinational prospective study, we did not find significant associations between unprocessed red meat and poultry intake and mortality or major CVD.
Controversy on the correlation of red and processed meat consumption with colorectal cancer risk: an Asian perspective (full paper)
by Sun Jin Hur, et al
We conducted an in-depth analysis of prospective, retrospective, case-control and cohort studies, systematic review articles, and IARC monograph reports, which revealed that the IARC/WHO report weighted the results of studies based in Western countries more and that the correlation between intake of processed meat products and colorectal cancer incidence in Asians is not clearly supported. Among 73 epidemiological studies, approximately 76% were conducted in Western countries, whereas only 15% of studies were conducted in Asia. Furthermore, most studies conducted in Asia showed that processed meat consumption is not related to the onset of cancer. Moreover, there have been no reports showing significant correlation between various factors that directly or indirectly affect colorectal cancer incidence, including processed meat products types, raw meat types, or cooking methods.
Red meat and colon cancer: A review of mechanistic evidence for heme in the context of risk assessment methodology
by Claire Kruger & Yuting Zhou
In conclusion, the methodologies employed in current studies of heme have not provided sufficient documentation that the mechanisms studied would contribute to an increased risk of promotion of preneoplasia or colon cancer at usual dietary intakes of red meat in the context of a normal diet.
Meat intake and cause-specific mortality: a pooled analysis of Asian prospective cohort studies
by Jung Eun Lee, et al
Ecological data indicate an increase in meat intake in Asian countries; however, our pooled analysis did not provide evidence of a higher risk of mortality for total meat intake and provided evidence of an inverse association with red meat, poultry, and fish/seafood. Red meat intake was inversely associated with CVD mortality in men and with cancer mortality in women in Asian countries.”
No association between meat intake and mortality in Asian countries
by Dominik D Alexander
After pooling data across the cohorts, Lee et al (3) observed no significant increases in risk of all-cause mortality comparing the highest with the lowest intake categories of total meat, red meat, poultry, or fish. In contrast, most associations were in the inverse direction with significant decreased risks for poultry (among men and women) and fish (women), with a nearly significant decreased risk with greater intakes of red meat in women (upper CI: 1.00). Similar patterns of associations (most indicating a decreased risk) were observed for cause-specific mortality; comparing the highest with the lowest intake categories, significant decreased risks of CVD mortality with red meat (men) and cancer mortality with red meat and poultry (women) were observed. The only significant positive association in the overall analyses was for the highest category of fish intake and cancer mortality. Little effect modification was apparent after stratification by educational level and by BMI.
Cancer link to red meat consumption may not exist for Asians: Study
by Pearly Neo
Researchers in Korea have discovered that the link between meat consumption and colorectal cancer may not apply to Asians. The meat-colorectal cancer correlation was first elucidated in a report by the International Agency for Research on Cancer (IARC) in 2015. The Korean researchers carried out a thorough review of over 500 studies that had previously been conducted on meat consumption and cancer. These included cohort and case-control analyses, prospective and retrospective studies, other review articles, as well as IARC monograph reports. Of these, 73 human epidemiological studies were selected for more in-depth analysis.
“The aim was to investigate the relationship between meat intake and colorectal cancer risk from an Asian, particularly Korean, perspective,” said the authors. “[We found] that approximately 76% [of the studies] were conducted in Western countries, whereas only 15% of studies were conducted in Asia. Furthermore, most studies conducted in Asia showed that processed meat consumption is not related to the onset of cancer.” “[As such], the correlation between intake of processed meat products and colorectal cancer incidence in Asians is not clearly supported,” they concluded. The study also reported that there do not exist any conclusive reports proving a significant correlation between meat consumption and colorectal cancer, whether it involves processed meats, raw meats or the relevant cooking methods.
Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations From the Nutritional Recommendations (NutriRECS) Consortium
by Bradley C. Johnston, et al
Recommendations: The panel suggests that adults continue current unprocessed red meat consumption (weak recommendation, low-certainty evidence). Similarly, the panel suggests adults continue current processed meat consumption (weak recommendation, low-certainty evidence). […]
Contemporary dietary guidelines recommend limiting consumption of unprocessed red meat and processed meat. For example, the 2015–2020 Dietary Guidelines for Americans recommend limiting red meat intake, including processed meat, to approximately 1 weekly serving (1). Similarly, United Kingdom dietary guidelines endorse limiting the intake of both red and processed meat to 70 g/d (2), and the World Cancer Research Fund/American Institute for Cancer Research recommend limiting red meat consumption to moderate amounts and consuming very little processed meat (3). The World Health Organization International Agency for Research on Cancer has indicated that consumption of red meat is “probably carcinogenic” to humans, whereas processed meat is considered “carcinogenic” to humans (4). “These recommendations are, however, primarily based on observational studies that are at high risk for confounding and thus are limited in establishing causal inferences, nor do they report the absolute magnitude of any possible effects. Furthermore, the organizations that produce guidelines did not conduct or access rigorous systematic reviews of the evidence, were limited in addressing conflicts of interest, and did not explicitly address population values and preferences, raising questions regarding adherence to guideline standards for trustworthiness (5–9). […]
In our assessment of causal inferences on unprocessed red meat and processed meat and adverse health outcomes, we found that the absolute effect estimates for red meat and processed meat intake (13, 16) were smaller than those from dietary pattern estimates (14), indicating that meat consumption is unlikely to be a causal factor of adverse health outcomes (Table 1).
Total Meat Intake is Associated with Life Expectancy: A Cross-Sectional Data Analysis of 175 Contemporary Populations
by Wenpeng You, et al
This ecological study examined the relationship between meat intake and life expectancy at birth e(0), at age 5 years e(5) and child mortality at a population level. Our statistical analysis results indicate that countries with the greater meat intake have greater life expectancy and lower child mortality. This relationship is independent of the effects of caloric intake, socioeconomic status (GDP PPP), obesity, urbanization (lifestyle) and education. Of course, nutritional variations among countries include many more variables than those included into this study. Diet composition, food preparation methods, cultural dietary constraints, availability of some nutrients and a number of other variables should have been considered to obtain a complete picture of meat’s importance in human diet. However, even with these possible analytical inadequacies, our statistical analyses indicate a significant role that meat plays in influencing variation of survival and mortality.
Meat has advantages over food of plant origin in containing complete protein with all essential amino acids, is rich in vitamins, in particular vitamin B12, and all essential minerals. It has a significant role not only for maintenance of health, development and proper growth59 but also has played an important evolutionary role in ancestral hominins for approximately 2.6 million years.60,61
Benefits of meat eating include better physical growth and development,62 optimal breastfeeding of neonates, and offspring growth.63 Human adaptation to meat eating and mechanism to digest and metabolise meat6,59,62,64–67 have been supported by studies in human dietary evolution. This may also be reflected in the importance of meat eating for human’s whole life span.5,60,68 Culturally, meat production and eating have also been integrated into human societies.62,69–72
A study of more than 218,000 adults from over 50 countries around the world suggests that consuming unprocessed meat regularly can reduce the risk of early death and can increase human longevity.73 A recent dietary advice published by Lancet Public Health advocates an increase of dietary meat in order to benefit our heart health and longevity.74 This study also highlights that saturated fat in meat may be cardio protective, as well as, that meat contains many vitamins and the essential amino acids for human health and well-being.73,74
Recent epidemiological literature highlights that increasing meat consumption, especially in its processed forms, may have adverse health effects, such as cancer,8 cardiovascular disease,75 obesity31,76–78 and diabetes.79 However, there has been no clinical trial evidence to consolidate the putative negative effects of processed meat consumption for human health.21 The aforementioned epidemiological literature is not reflected in the healthy food guidelines published by the government authorities for general public. These guidelines always include meat as a major human dietary component. One reason for their position could be a lack of evidence-based research that demonstrates negative aspects of meat consumption in the general human population.80–83 Statistically, the finding of this study unequivocally indicates that meat eating benefits life expectancy independently.
Meat contains high protein with all the essential amino acids, and is a good source of minerals (iron, phosphorus, selenium and zinc) and vitamins (B12, B6, K, choline, niacin, riboflavin). Simply put – a human animal consuming a body of another animal gets practically all constituent compounds of its own body.
Behavioral Characteristics and Self-Reported Health Status among 2029 Adults Consuming a “Carnivore Diet”
by Belinda S Lennerz, et al
(also see: Reply to R Kirwan, GS Mallett, L Ellis, and A Flanagan)
In this social media–based survey, a self-selected group of adults consuming a carnivore diet for ≥6 mo reported perceived good health status, perceived absence of symptoms of nutritional deficiencies, and high satisfaction with this eating pattern. To our knowledge, this is the first modern report on a large group of people habitually consuming few plant foods, a dietary pattern broadly considered incompatible with good health.
Weight loss and other health benefits were most frequently indicated as the motivation for adoption of a carnivore diet. In accordance with this possibility, respondents reported substantial BMI reduction and improvements in physical and mental well-being, overall health, and numerous chronic medical conditions. Respondents with diabetes reported special benefit, including greater weight loss than the overall group, and marked reductions in diabetes medication usage and HbA1c—notable findings in view of the generally low success of lifestyle interventions for obesity and diabetes (37, 38). Although we did not formally assess macronutrient intake, carbohydrate content in meat and other animal-based foods is minimal, and inherent limits to protein intake exist. Both ancestral data (39) and self-reported preference of fatty cuts of meat in our survey suggest high fat intake with the carnivore diet. As such, the macronutrient composition of a carnivore diet would likely correspond to other very-low-carbohydrate diets (e.g., ketogenic, Atkins). For this reason, studies of these diets may provide relevant comparisons. In meta-analyses of trials for T2DM, low- compared with high-carbohydrate diets produced greater weight loss (40–42), lower HbA1c (40–46), and reduction in usage of glucose-lowering medications (41, 43, 45, 46), consistent with our observations. Although general dietary adherence and glycemic effects diminish over time (47), the findings of 1 recent nonrandomized trial suggest that a very-low-carbohydrate diet may be sustainable and efficacious when combined with high-intensity individual support (48).
Consistent with other low-carbohydrate diet studies (40–45), respondents reported a mixed blood lipid pattern: LDL-cholesterol, a major conventional cardiovascular disease risk factor, was markedly elevated whereas HDL-cholesterol and TG were favorable. However, LDL-cholesterol elevation, when associated with low TG, may reflect large, buoyant lipoprotein particles, possibly comprising a relatively low-risk subtype (49). Indeed, the low ratio of TG to HDL-cholesterol is suggestive of high insulin sensitivity and good cardiometabolic health (50). However, it is unclear whether this apparent benefit of the diet, together with the reported weight reduction and improved glycemic control (in the subset with diabetes), would counterbalance or outweigh any increased risk from LDL-cholesterol elevation. For individuals with a more extreme LDL-cholesterol response, drug treatment could be considered—an option that is generally more effective and better tolerated than drug treatment of insulin-resistance dyslipidemia.
Beyond macronutrient composition, elimination of allergenic, inflammatory, or other food components may provide potential health benefits to individuals following a carnivore diet. Food allergies and sensitivities are common, and predominantly related to plant foods (51). Some plant chemicals may produce adverse effects through other mechanisms, such as lecithin in beans, cyanogenic glycosides in certain seeds, and glycoalkaloids in potatoes. Indeed, >50% of survey participants started the carnivore diet to improve allergic, skin, or autoimmune conditions, or digestive health, and many reported improvements in inflammatory conditions and related symptoms. Conversely, dietary intake may be low for vitamins that are typically derived from plant foods (e.g., fruits, vegetables, nuts, seeds, and grains) or from nutritional fortification of staple foods (e.g., milk, juices, cereals, pastas, and other grain products) (52, 53). In addition, often unquantified phytochemicals (e.g., polyphenols, alkylresorcinols, phytosterols) are largely absent from the diet. Although these phytochemicals do not have DRIs, they have been linked to cardiometabolic benefits (54, 55). In people who eat meat only with exclusion of dairy (∼30% in this survey), calcium intake might also be low, as illustrated by the low intake and negative calcium balance in 2 Arctic explorers (28). Although essential nutrients can presumably be derived in sufficient amounts from animal foods (34), they are present in less commonly consumed parts of the animal, such as fat and organ meats (vitamins A and D), or bone (calcium), or may be reduced during food preparation (vitamin C) (34). Vitamin C is of particular interest, because meats are not formally considered a good source of vitamin C (i.e., they contain <10% of the DRI per serving) (56). Typical symptoms of deficiencies in these vitamins would include dermatological, cognitive, or neurological symptoms, as listed in Supplemental Table 1. A worsening or new presentation of these symptoms was reported in <2% of survey participants, whereas the majority of participants reported improvements, resolution, or no change—regardless of intake of vitamins, organ meat, or dairy. Given the self-reported nature of these findings, it remains unclear whether clinical or subclinical symptoms of nutrient deficiency are present. Research is needed to clarify the absence of perceived symptoms of nutrient deficiencies and the underlying biochemical processes that govern nutrient needs with the long-term consumption of a carnivore diet. It is possible that requirements for some micronutrients may be lower than those established in DRIs for the general population (57), related to remodeling of the gut microbiome, whole-body metabolism, and nutrient utilization in the setting of a low-carbohydrate carnivore diet, analogous to observations with a vegan diet (58).
Respondents reported high levels of satisfaction, and little social impact, from following a carnivore diet. Notably, medical providers were perceived as supportive, neutral, or unsupportive at generally similar proportions despite the discrepancy of the carnivore diets from dietary guidelines. Whereas meat is more expensive than grains and starchy foods, it may be less expensive on a caloric basis, depending on location and specific comparisons, than fresh fruits and nonstarchy vegetables (59), and cost may be in addition offset by decreased expenditure for diabetes and other medications. Our respondents spanned low to high income classes, suggesting against major financial barriers to the diet.
Vegetarians and Heart Disease: Will Ditching Meat Really Save Your Arteries?
by Denise Minger
Studies on vegetarians are inherently tricky. Although some folks dump animal foods strictly for ethical reasons, many of the meatless [Maria Gacek, Selected lifestyle and health condition indices of adults with varied models of eating] eat their veggies alongside other pro-health behaviors like exercising more, nixing tobacco, swapping refined grains for whole, limiting processed food (soy Frankenmeats notwithstanding), and avoiding the biggest of the baddies (trans fats, corn syrup, Cadbury Creme Eggs, and pretty much everything on this site).
What does all of that equal? Confounderville for researchers. It’s impossible to adjust for every little diet and lifestyle tweak a vegetarian makes in the name of health, so in scientific studies, vegetarians almost always have an advantage over health-indifferent omnivores. But the reason can’t be pegged on their meatlessness: Vegetarianism is a marker for a comprehensive shift in behaviors that influence disease risk.
But that’s not always the case with all groups of vegetarians. Studies focusing on some religious vegetarians (namely Buddhist and Hindu*) are more likely to show the effects of going meat-free in isolation rather than as part of a health-boosting plan. Confounding can still be an issue (especially in terms of stress reduction from certain religious practices)—but unlike the vegetarians who make a cascade of changes when they ditch meat, some religious vegetarians eat diets pretty similar to their omnivorous counterparts, just without flesh. That makes it a bit easier to compare apples with apples: We can see how an average omni diet stacks up against a similar diet sans meat, instead of comparing an average omni diet with a multifaceted vegetarian lifestyle.
So where am I going with this? Right here [Chih-Wei Chen et al, Taiwanese Female Vegetarians Have Lower Lipoprotein-Associated Phospholipase A2 Compared with Omnivores]. That’s the full text for a recent study from Taiwan looking at inflammatory markers in mostly-Buddhist vegetarians versus omnivores. (And if access to that link disappears, as full-texts are wont to do, just shoot me an email and I’ll send it to you.)
This study has a few good things going for it. For starters, it excludes smokers and uses only women—which automatically eliminates problems associated with controlling for tobacco use or gender-related differences in inflammatory markers. As the researchers note, the health-consciousness gap between Taiwanese vegetarians and Taiwanese omnivores is probably much smaller than with Western vegetarians and Western omnivores:
Most western vegetarians include fresh vegetables and fruits as their main source of nutrition and energy, based on health benefits of the foods. In contrast, most Taiwanese vegetarians choose a vegetarian diet because of their Buddhist religion, which teaches a policy of “no killing.” Buddhists in Taiwan have a dietary pattern similar to that of most Taiwanese in terms of meal patterns and cooking methods, except that they do not include any meat, fish, or poultry in their meals.
Although the researchers don’t explore the subject at all, the difference in religious practices between the vegetarians (apparently Buddhist) and omnivores (whose religion(s) weren’t documented) could be significant. Stress and mental outlook may play a role [K Rees et al, Psychological interventions for coronary heart disease] in the progression of heart disease, and meditation/centering practices associated with Buddhism could help improve both [Erin L Olivo et al, Feasibility and effectiveness of a brief meditation-based stress management intervention for patients diagnosed with or at risk for coronary heart disease: a pilot study]. If any of that is confounding the results, we won’t be able to know from the data presented.
But other than that, the study was pretty thorough. It tracked BMI, blood pressure, heart rate, glucose levels, cholesterol (total, HDL, and LDL), white blood cell count, homocysteine, and two inflammatory markers: lipoprotein-associated phospholipase AS (Lp-PLA2) and C-reactive protein (CRP).
The good news for the vegetarians is that their Lp-PLA2—a marker specifically for vascular inflammation—was lower than in the control group. But that’s where the good news ends. The researchers seemed pretty surprised to report that the vegetarians had higher levels of CRP (borderline significant at p=0.05) than the omnivores, along with higher homocysteine and triglycerides. […]
Interestingly, the researchers note that one of their earlier studies [C-W Chen et al, Total cardiovascular risk profile of Taiwanese vegetarians] showed borderline lower CRP in vegetarians—but despite using it to claim vegetarians had a better risk profile than omnivores, that finding might not be very meaningful:
As we know, gender and smoking influenced the serum hs-CRP level significantly. In our previous study, there are more males and smokers in the omnivore group that can influence the statistical power of difference of hs-CRP between both groups. Actually, it failed to demonstrate a significant difference if male and female samples were analyzed separately.
In the current study, the researchers offer a few explanations as to why vegetarians might have higher CRP levels, even if their Lp-PLA2 levels were lower. One is that there were large variations in the CRP levels for all groups, which makes it harder to analyze statistically (translation: “maybe the correlation is a fluke”). They also mention that Taiwan vegetarians rely heavily on soy products as a substitute for meat, eat fewer fresh vegetables than western vegetarians, and typically cook vegetables in oil (presumably industrial seed oils).
The significance of this study is that it underscores the major issue with vegetarian research at large: The health-protective effects of vegetarianism are probably due to factors other than meat avoidance. When you study vegetarians that aren’t partaking in a bigger diet and lifestyle change, they no longer have a glowing health report. The lower Lp-PLA2 levels in this particular study are noteworthy, but higher CRP and triglycerides aren’t doing anyone any favors.
Of course, this isn’t the first study to poke holes the claim that meat-avoiders have special protection against heart disease. A 2005 study conducted in China [Timothy Kwok et al, Vascular Dysfunction in Chinese Vegetarians: An Apparent Paradox?] rounded up some long-term vegetarians (6 to 40 years of meatlessness)—including many religious vegetarians—and compared their heart disease markers against an omnivorous control group. Apart from eating less saturated fat, protein, and cholesterol, the vegetarians had nutrient intakes similar to those of their omni friends.
The surprising results? The vegetarians had significantly thicker arterial walls (p<0.0001), reduced flow-mediated dilation (a predictor of cardiovascular events) (p<0.0001), higher blood pressure (p<0.05), and higher triglycerides (p<0.05) than the omnivores. (According to the paper, the raised blood pressure might be related to some popular high-sodium vegetarian foods such as processed protein food substitutes, fake oyster sauce, and tomato paste.)
In the researchers’ multivariate statistical models, vegetarianism had the strongest association with both artery thickness and diminished flow-mediated dilation out of all the variables documented—including age, gender, and triglyceride levels.
As might be expected, the vegetarians also had lower B12 levels and higher homocysteine than the control group—but even after adjusting for these, vegetarianism remained strongly linked with less-healthy hearts. The researchers concluded with this:
In summary, contrary to common belief, vegetarians, at least in the Chinese, might have accelerated atherosclerosis and abnormal arterial endothelial function, compared with omnivore control subjects. The increased risk could only be partially explained by their higher blood pressure, triglyceride, homocysteine, and lower vitamin B12 concentrations.
A little alarming, no? My guess is that these vegetarians got such a lousy report card because they didn’t make all the positive health changes most Western vegetarians make when they forgo flesh—but rather, replaced meat with processed foods, ate more carbohydrates and polyunsaturated plant fats, and failed to get enough B12 (resulting in higher homocysteine). This is what happens when you simply pluck meat out of your diet and fill the void with plant-based substitutes: the Healthy Vegetarian image becomes a lot less rosy.
No doubt some vegetarians would dismiss this study because the participants “did vegetarianism wrong” by not supplementing B12, not eating enough fruit and vegetables, consuming too much salt, and failing to provide daily offerings to the Arugula God. But if that’s the case, one could argue that all the meat eaters in the studies supporting vegetarianism just “did omnivorism wrong” for similar reasons. This is a good study because neither the vegetarians nor the omnivores seemed particularly health conscious. It’s rare that we get a level playing field like that.
Should dietary guidelines recommend low red meat intake?
by Frédéric Leroy & Cofnas
3. Meat eating and chronic disease: evaluation of the evidence
3.1. Evidence from observational studies needs to be interpreted with care
As a first point of concern, the input data obtained from food frequency questionnaires should be interpreted prudently as they can be problematic for a variety of reasons (Schatzkin et al., 2003; Archer et al., 2018; Feinman, 2018). Social desirability bias in food reporting is just one example, as reported consumption can be affected by the perceived health status of certain foods. Not all self-defined vegetarians avoid meat, which is suggestive of a considerable risk for underreported intake in health-conscious groups (Haddad & Tanzman, 2003).
Secondly, diets are difficult to disentangle from other lifestyle factors. It has been shown that Western-style meat eating is closely associated with nutrient-poor diets, obesity, smoking, and limited physical activity (Alexander et al., 2015; Fogelholm et al., 2015; Grosso et al., 2017; Turner & Lloyd, 2017). Given the fact that health authorities have been intensely promoting the view that meat is unhealthy, health-conscious people may be inclined to reduce intake. Typically, the associations between meat eating and disease tend to be higher in North American than in European or Asian cohort studies, indicating the presence of lifestyle bias and the need for cross-cultural assessments (Wang et al., 2016; Grosso et al., 2017; Hur et al., 2018). A pooled analysis of prospective cohort studies in Asian countries even indicated that red meat intake was associated with lower cardiovascular mortality in men and cancer mortality in women (Lee et al., 2013). Likewise, when omitting Seventh-Day Adventist studies from meta-analyses, the beneficial associations with cardiovascular health for vegetarian diets are either less pronounced or absent indicating the specific effects of health-conscious lifestyle rather than low meat consumption as such (Kwok et al., 2014; FCN, 2018). This is important, as Seventh-Day Adventism has had considerable influence on dietary advice worldwide (Banta et al., 2018).
As a third point, the relative risks (RRs) obtained from observational studies are generally low, i.e., much below 2. In view of the profusion of false-positive findings and the large uncertainty and bias in the data due to the problems mentioned above (Boffetta et al., 2008; Young & Karr, 2011), such low RR levels in isolation would not be treated as strong evidence in most epidemiological research outside nutrition (Shapiro, 2004; Klurfeld, 2015). Relationships with RRs below 2, which are susceptible to confounding, can be indicative but should always be validated by other means, such as randomized controlled trials (RCTs) (Gerstein et al., 2019). The association between meat eating and colorectal cancer, for instance, leads to an RR estimate below 1.2, whereas for the association between visceral fat and colorectal neoplasia this value equals 5.9 (Yamamoto et al., 2010). The latter provides a robust case that is much more deserving of priority treatment in health policy development. […]
3.2. Intervention studies have not been able to indicate unambiguous detrimental effects
As stated by Abete et al. (2014), epidemiological findings on meat eating “should be interpreted with caution due to the high heterogeneity observed in most of the analyses as well as the possibility of residual confounding”. The interactions between meat, overall diet, human physiology (including the gut microbiome), and health outcomes are highly intricate. Within this web of complexity, and in contrast to what is commonly stated in the public domain (Leroy et al., 2018a), the current epidemiological and mechanistic data have not been able to demonstrate a consistent causal link between red meat intake and chronic diseases, such as colorectal cancer (Oostindjer et al., 2014; Turner & Lloyd, 2017).
RCTs can play an important role in establishing causal relationships, and generally provide much stronger evidence than that provided by observational data. However, even RCTs are not fail-safe and can also be prone to a range of serious flaws (Krauss, 2018). Intervention studies that overlook the normal dietary context or use non-robust biomarkers should be interpreted with caution, and do not justify claims that there is a clear link between meat and negative health outcomes (see Turner & Lloyd, 2017; Kruger & Zhou, 2018). The available evidence generally suggests that interventions with red meat do not lead to an elevation of in vivo oxidative stress and inflammation, which are usually cited as being part of the underlying mechanisms triggering chronic diseases (Mann et al., 1997; Hodgson et al., 2007; Turner et al., 2017). Even in an epidemiological cohort study that was suggestive of an inflammatory response based on an increased CRP level, this effect became non-significant upon adjustment for obesity (Montonen et al., 2013). Moreover, a meta-analysis of RCTs has shown that meat eating does not lead to deterioration of cardiovascular risk markers (O’Connor et al., 2017). The highest category of meat eating even paralleled a potentially beneficial increase in HDL-C level. Whereas plant-based diets indeed seem to lower total cholesterol and LDL-C in intervention studies, they also increase triglyceride levels and decrease HDL-C (Yokoyama et al., 2017), which are now often regarded as superior markers of cardiovascular risk (Jeppesen et al., 2001).
Based on the above, we conclude that there is a lack of robust evidence to confirm an unambiguous mechanistic link between meat eating as part of a healthy diet and the development of Western diseases. It is paramount that the available evidence is graded prior to developing policies and guidelines, making use of quality systems such as GRADE (Grading of Recommendations Assessment, Development and Evaluation; Guyatt et al., 2008). One of the founders of the GRADE system has issued a public warning that the scientific case against red meat by the IARC panel of the WHO has been overstated, doing “the public a disservice” (Guyatt, 2015). The IARC’s (2015) claim that red meat is “probably carcinogenic” has never been substantiated. In fact, a risk assessment by Kruger and Zhou (2018) concluded that this is not the case. Such hazard classification systems have been heavily criticized, even by one of the members of the IARC working group on red meat and cancer (Klurfeld, 2018). They are accused of being outmoded and leading to avoidable health scares, public funding of unnecessary research and nutritional programs, loss of beneficial foods, and potentially increased health costs (Boyle et al., 2008; Anonymous, 2016; Boobis et al., 2016).
3.3. A scientific assessment should not overlook conflicting data
Dietary advice that identifies meat as an intrinsic cause of chronic diseases often seems to suffer from cherry-picking (Feinman, 2018). One example of a fact that is typically ignored is that hunter-gatherers are mostly free of cardiometabolic disease although animal products provide the dominant energy source (about two-thirds of caloric intake on average, with some hunter-gatherers obtaining more than 85% of their calories from animal products; Cordain et al., 2000, 2002). In comparison, contemporary Americans obtain only about 30% of calories from animal foods (Rehkamp, 2016).
Whereas per capita consumption of meat has been dropping over the last decades in the US, cardiometabolic diseases such as type-2 diabetes have been rapidly increasing. Although this observation does not resolve the question of causality one way or the other, it should generate some skepticism that meat is the culprit (Feinman, 2018). Moreover, several studies have found either that meat intake has no association with mortality/morbidity, or that meat restriction is association with various negative health outcomes (e.g., Key et al., 2009; Burkert et al., 2014; Kwok et al., 2014; Lippi et al., 2015; Hur et al., 2018; Iguacel et al., 2018; Yen et al., 2018). As another example of conflicting information, the epidemiological association pointing to a potential role of the meat nutrient L-carnitine in atherosclerosis via trimethylamine N-oxide (TMAO) formation (Koeth et al., 2013), is contradicted by intervention studies (Samulak et al., 2019) and epidemiological data showing that fish intake, being by orders of magnitude the largest supplier of TMAO (Zhang et al., 1999), improves triglycerides and HDL levels (Alhassan et al., 2017). […]
5. Meat avoidance leads to a loss of nutritional robustness
Diets poor in animal source foods can lead to various nutritional deficiencies, as already described more than a century ago for the case of pellagra (Morabia, 2008), a condition which remains relevant today for poorly planned vegan diets (Ng & Neff, 2018). Advocates of vegetarian/vegan diets usually admit that these diets must indeed be “well-planned” in order to be successful, which involves regular supplementation with nutrients such as B12. However, realistically, many people are not diligent about supplementation, and will often dip into deficient or borderline-deficient ranges if they do not obtain nutrients from their regular diet. In such cases, general malnutrition (Ingenbleek & McCully, 2012), poorer health (Burkert et al., 2014), and nutrient limitations (Kim et al., 2018) may be the result, as found in various countries, such as Denmark (Kristensen et al., 2015), Finland (Elorinne et al., 2016), Sweden (Larsson & Johansson, 2002), and Switzerland (Schüpbach et al., 2017). For example, a substantial number of vegetarians and vegans are in the deficient or borderline-deficient range for B12 (Herrmann & Geisel, 2002; Herrmann et al., 2003), despite the fact that the need for B12 supplementation is well-publicized (see also Herbert, 1994; Hokin & Butler, 1999; Donaldson, 2000; Elmadfa & Singer, 2009; Gilsing et al., 2010; Obersby et al., 2013; Pawlak et al. 2013, 2014; Pawlak, 2015; Woo et al., 2014; Naik et al., 2018). B12 deficiency is particularly dangerous during pregnancy (Specker et al., 1988, 1990; Bjørke Monsen et al., 2001; Koebnick et al., 2004), childhood (Rogers et al., 2003) and adolescence (van Dusseldorp et al., 1999; Louwman et al., 2000).
Other potentially challenging micronutrients for people on plant-based diets include (but are not limited to) iodine (Krajcovicová-Kudlácková et al., 2008; Leung et al., 2011; Brantsaeter et al., 2018), iron (Wilson & Ball, 1999; Wongprachum et al., 2012; Awidi et al., 2018), selenium (Schultz & Leklem, 1983; Kadrabová et al., 1995), and zinc (Foster et al., 2013). Even if plant-based diets contain alpha linolenic acid, this may not (as noted) prevent deficiencies in the long-chain omega-3 fatty acids EPA and DHA (Rosell et al., 2005), which can pose serious risks in pregnancy and for growing children (Burdge et al., 2017; Cofnas, 2019).
Risks of nutritional deficiency are also documented by an extensive list of clinical case reports in the medical literature, with serious and sometimes irreversible pathological symptoms being reported for infants (e.g., Shinwell & Gorodisher, 1982; Zengin et al., 2009; Guez et al., 2012; Bravo et al., 2014; Kocaoglu et al., 2014; Goraya et al., 2015), children (e.g., Colev et al., 2004; Crawford & Say, 2013), adolescents (e.g., Chiron et al., 2001; Licht et al., 2001; O’Gorman et al., 2002), and adults (e.g., Milea et al., 2000; Brocadello et al., 2007; De Rosa et al., 2012; Førland & Lindberg, 2015). The latter reports commonly refer to failure to thrive, hyperparathyroidism, macrocytic anemia, optic and other neuropathies, lethargy, degeneration of the spinal cord, cerebral atrophy, and other serious conditions. Although the direction of causality is not clear, meat avoidance is statistically associated with eating disorders and depression (Zhang et al., 2017; Barthels et al., 2018; Hibbeln et al., 2018; Matta et al., 2018; Nezlek et al., 2018) and may mirror neurological problems (Kapoor et al., 2017).
Our main concern is that avoiding or minimizing meat consumption too strictly may compromise the delivery of nutrients, especially in children and other vulnerable populations. Evidently, health effects of plant-based approaches depend largely on the dietary composition (Satija et al., 2016). Yet, the more restricted the diet and the younger the age, the more this will be a point of attention (Van Winckel et al., 2011). According to Cofnas (2019), however, even realistic vegetarian diets that include diligent supplementation can put children at risk for deficiencies and thereby compromise health in both the short and long term. There is some direct and indirect evidence that the elevated phytoestrogen intake associated with low-meat diets may pose risks for the development of the brain and reproductive system (Cofnas, 2019). Moreover, attempts to introduce dietary modifications that are also compatible with vegan philosophy often pose a medicosocial challenge (Shinwell & Gorodischer, 1982). In our opinion, the official endorsement of diets that avoid animal products as healthy options is posing a risk that policy makers should not be taking. As stated by Giannini et al. (2006): “It is alarming in a developed country to find situations in which a child’s health is put at risk by malnutrition, not through economic problems but because of the ideological choices of the parents”.
* * *
On the China Study:
To explore a specific area of debate, consider Colin Campbell’s book The China Study. It was a correlative analysis of earlier data. And it’s focus on an Asian population is relevant. But some have pointed out that the correlations are mostly statistically non-significant while other statistically significant correlations were ignored. The best and most thorough critique was done by Denise Minger, in a series of articles she published at her website. One of her articles was specifically about the meat issue. Even one of the original researchers admitted that nothing meaningful was likely to be concluded from the data because there simply is too much noise of uncontrolled confounders. Anyway, in summarizing some of Minger’s findings, Harriet Hall wrote,
“The data do show that cholesterol is positively associated with various cancers, that cholesterol is positively associated with animal protein, and that cholesterol is negatively associated with plant protein. So by indirect deduction they assume that animal protein is associated with cancers and that reducing intake is protective. But if you compare animal protein intake directly with cancer, there are as many negative correlations as positive, and not one of those correlations reaches a level of statistical significance. Comparing dietary plant protein to various types of cancer, there are many more positive correlations and one of them does show strong statistical significance. The variable “death from all cancers” is four times as strongly associated with plant protein as with animal protein. And Campbell fails to mention an important confounder: cholesterol is higher in geographic areas with a higher incidence of schistosomiasis and hepatitis B infection, both risk factors for cancer.
“Campbell says breast cancer is associated with dietary fat (which is associated with animal protein intake). The data show a non-significant association with dietary fat, but stronger (still non-significant) associations with several other factors and a significant association with wine, alcohol, and blood glucose level. The (non-significant) association of breast cancer with legume intake is virtually identical to the (non-significant) association with dietary fat. Animal protein itself shows a weaker correlation with breast cancer than light-colored vegetables, legume intake, fruit, and a number of other purportedly healthy plant foods.)
“He indicts animal protein as being correlated with cardiovascular disease, but fails to mention that plant protein is more strongly correlated and wheat protein is far, far more strongly correlated. The China Study data show the opposite of what Campbell claims: animal protein doesn’t correspond with more disease, even in the highest animal food-eating counties” (The China Study Revisited: New Analysis of Raw Data Doesn’t Support Vegetarian Ideology).
Beyond Minger, others have also responded to The China Study that gets cited endlessly by vegans. Chris Kresser noted that, “Campbell conveniently fails to mention the county of Tuoli in China. The folks in Tuoli ate 45% of their diet as fat, 134 grams of animal protein each day (twice as much as the average American), and rarely ate vegetables or other plant foods. Yet, according to the China Study data, they were extremely healthy with low rates of cancer and heart disease; healthier, in fact, than many of the counties that were nearly vegan” (Rest in Peace, China Study). Another Chris, of the Masterjohn variety, discussed issues involving the roles of lysine and folate, with his giving credit to Minger for making the connection to lysine (Denise Minger’s Refutation of Campbell’s “China Study” Generates Continued Debate).
* * *
Research on non-meat animal foods and saturated fat:
‘Dietary guidelines are likely wrong’: Saturated fat does not increase cardiovascular disease risk, argue researchers
by Flora Southey
Aren’t Saturated Fats Bad For You?
by Dr. Nicholas Norwitz
The Scientific Evidence On Saturated Fats
from Nutrition Coalition
(This is a collection of studies and reviews, far beyond what is included here.)
In order to continue the limits on saturated fat, health officials must show ample and consistent evidence that these fats damage health. The principal allegation against them has been that they cause heart disease, according to the diet-heart hypothesis which was first proposed in the 1950s.[1]
Many large, government-funded RCTs (randomized, controlled clinical trials, which are considered the ‘gold-standard’ of science) were conducted all over the world in the 1960s and 70s in order to test the diet-heart hypothesis. Some 75,000 people were tested, in trials that on the whole followed subjects long enough to obtain “hard endpoints,” which are considered more definitive than LDL-C, HDL-C, etc. However, the results of these trials did not support the hypothesis, and consequently, they were largely ignored or dismissed for decades—until scientists began rediscovering them in the late 2000s. The first comprehensive review of these trials was published in 2010 and since then, there have been nearly 20 such review papers, by separate teams of scientists all over the world.
Saturated fat: villain and bogeyman in the development of cardiovascular disease?
by Reimara Valk, James Hammill, & Jonas Grip (PDF)
Results: Collectively, neither observational studies, prospective epidemiologic cohort studies, RCTs, systematic reviews and meta analyses have conclusively established a significant association between SFA in the diet and subsequent cardiovascular risk and CAD, MI or mortality nor a benefit of reducing dietary SFAs on CVD rick, events and mortality. Beneficial effects of replacement of SFA by polyunsaturated or monounsaturated fat or carbohydrates remain elusive.
Conclusions: Findings from the studies reviewed in this paper indicate that the consumption of SFA is not significantly associated with CVD risk, events or mortality. Based on the scientific evidence, there is no scientific ground to demonize SFA as a cause of CVD. SFA naturally occurring in nutrient-dense foods can be safely included in the diet.
United States Dietary Trends Since 1800: Lack of Association Between Saturated Fatty Acid Consumption and Non-communicable Diseases
by Joyce H. Lee, Miranda Duster, Timothy Roberts, & Orrin Devinsky
Methods: We examined food availability and estimated consumption data from 1800 to 2019 using historical sources from the federal government and additional public data sources.
Results: Processed and ultra-processed foods increased from <5 to >60% of foods. Large increases occurred for sugar, white and whole wheat flour, rice, poultry, eggs, vegetable oils, dairy products, and fresh vegetables. Saturated fats from animal sources declined while polyunsaturated fats from vegetable oils rose. Non-communicable diseases (NCDs) rose over the twentieth century in parallel with increased consumption of processed foods, including sugar, refined flour and rice, and vegetable oils. Saturated fats from animal sources were inversely correlated with the prevalence of NCDs.
Conclusions: As observed from the food availability data, processed and ultra-processed foods dramatically increased over the past two centuries, especially sugar, white flour, white rice, vegetable oils, and ready-to-eat meals. These changes paralleled the rising incidence of NCDs, while animal fat consumption was inversely correlated.
What Are The Functions of MCTs in Goat Milk?
from Aurora Health
The Health Benefits of Medium Chain Triglycerides in Goat Milk
by Sarah Holvik
Cow’s Milk and Dairy Consumption: Is There Now Consensus for Cardiometabolic Health?
by Sally D. Poppitt
Organic Whole Milk Is Better than Conventional Skim or Whole Milk, Studies Find
by Clarence Bass
In further support, Dr. Donald R. Davis, a co-author of the Benbrook study, pointed out that many now question the assumption that the saturated fat in whole milk increases the risk of cardiovascular disease. As this was being written a meta-analysis by Cambridge and Harvard Universities of 72 studies with 600,000 participants found no evidence that saturated fat is associated with a greater risk of heart disease (March 17, 2014, Annals of Internal Medicine). The new emphasis seems to be on eating a balanced diet of real foods, whole foods—and avoiding highly processed foods. (More about this next month.)
Do Not Give Young Children Plant-Based Milk, As It Lacks Important Nutrients, Pediatricians Warn
by Martha Garcia
Several childhood health organizations are warning that plant-based milk alternatives should not be consumed by children, as they lack key nutrients.
Young children under the age of five should only drink cows’ milk, water, and a minimal amount of juice each day, according to pediatric experts, who warn that children should avoid plant-based milk and other beverages that do not provide growing children with the nutrients they need for proper development.
These recommendations were made in the “Healthy Beverage Consumption in Early Childhood” September 2019 consensus statement, issued Wednesday as part of the Healthy Eating Research guidelines.
The statement was developed by a committee of leading health organizations, including a panel of experts with the Academy of Nutrition and Dietetics, the American Academy of Pediatric Dentistry, the American Academy of Pediatrics, and the American Heart Association.
The recommendations also indicate infants should only drink breast milk or infant formula. At six months of age, they can have small amounts of water, and after one year, they should only drink cows milk daily and occasionally juice.
The key change in this year’s guidelines was the call for young children to avoid plant-based milk. This includes milk made from rice, coconut, oats, almonds, or other blends, with the exception of fortified soy milk. Plant-based milks do not have the proper nutrition for early development, like vitamin D and calcium the experts said.
The Full-Fat Paradox: Whole Milk May Keep Us Lean
by Allison Aubrey
Consider the findings of two recent studies that conclude the consumption of whole-fat dairy is linked to reduced body fat.
In one paper, published by Swedish researchers in the Scandinavian Journal of Primary Health Care, middle-aged men who consumed high-fat milk, butter and cream were significantly less likely to become obese over a period of 12 years compared with men who never or rarely ate high-fat dairy.
Yep, that’s right. The butter and whole-milk eaters did better at keeping the pounds off.
“I would say it’s counterintuitive,” says Greg Miller, executive vice president of the National Dairy Council.
The second study, published in the European Journal of Nutrition, is a meta-analysis of 16 observational studies. There has been a hypothesis that high-fat dairy foods contribute to obesity and heart disease risk, but the reviewers concluded that the evidence does not support this hypothesis. In fact, the reviewers found that in most of the studies, high-fat dairy was associated with a lower risk of obesity.
“We continue to see more and more data coming out [finding that] consumption of whole-milk dairy products is associated with reduced body fat,” Miller says.
It’s not clear what might explain this phenomenon. Lots of folks point to the satiety factor. The higher levels of fat in whole milk products may make us feel fuller, faster. And as a result, the thinking goes, we may end up eating less.
Or the explanation could be more complex. “There may be bioactive substances in the milk fat that may be altering our metabolism in a way that helps us utilize the fat and burn it for energy, rather than storing it in our bodies,” Miller says.
In defense of dairy fat
by Allison Aubrey
A new study finds the dairy fats found in milk, yogurt and cheese may help protect against Type 2 diabetes.
The research, published in the journal Circulation, included 3,333 adults. Beginning in the late 1980s, researchers took blood samples from the participants and measured circulating levels of biomarkers of dairy fat in their blood. Then, over the next two decades, the researchers tracked who among the participants developed diabetes. “People who had the most dairy fat in their diet had about a 50 percent lower risk of diabetes” compared with people who consumed the least dairy fat, says Dariush Mozaffarian, dean of the Friedman School of Nutrition Science and Policy at Tufts University, who is also an author of the study. […]
“It appears that children who have a higher intake of whole milk or 2 percent milk gain less weight over time” compared with kids who consume skim or nonfat dairy products, explains DeBoer.
And there’s some evidence that dairy fat may help adults manage weight as well. As we’ve reported, researchers in Sweden found that middle-aged men who consumed high-fat milk, butter and cream were significantly less likely to become obese over a period of 12 years compared with men who never or rarely ate high-fat dairy. So, in other words, the butter and whole-milk eaters did better at keeping the pounds off. In addition, a meta-analysis –– which included data from 16 observational studies — also found evidence that high-fat dairy was associated with a lower risk of obesity. […]
And there’s evidence that “when people consume more low-fat dairy, they eat more carbohydrates” as a way of compensating, says Mozaffarian.
Many high-carb foods such as cereals, breads and snacks that contain highly refined grains are less satiating and can prompt people to eat more calories.
Plant-Based Milk Beverages Affect Children’s Height
by Ross Tellam
The investigators concluded that for the average child, each cup of noncow’s milk consumed per day was associated with a height decrease of 0.4 cm [1]. The investigators also concluded that the effect of the noncow’s milk beverages on height was not just due to the removal of the positive benefits of cow’s milk from the diet, i.e. consumption noncow’s milk was associated with the height loss. The height reduction at three years of age for the average child drinking three cups per day of noncow’s milk compared with the average child drinking three cups of cow’s milk was 1.5 cm.
Maguire and colleagues speculated that many noncow’s milk beverages may have reduced protein content compared with cow’s milk, which could explain the height decrease in the group consuming noncow’s milk. Other studies additionally suggest that plant-based milk proteins, unlike animal proteins, often do not contain all the essential amino acids required for optimal human growth and development [12–14]. The investigators further suggested that consumption of noncow’s milk by children may not induce increased levels of a natural growth promotant (insulin-like growth factor 1) as happens with the consumption of cow’s milk.
1. Morency M.E., Birken C.S., Lebovic G., Chen Y., L’Abbé M., Lee G.J., et al. Association between noncow milk beverage consumption and childhood height. Am J Clin Nutr. 2017;106(2):597-602.
* * *
Related posts:
Dietary Risk Factors for Heart Disease and Cancer
Blue Zones Dietary Myth
Eat Beef and Bacon!
Like water fasts, meat fasts are good for health.
Dr. Saladino on Plant and Animal Foods
Gundry’s Plant Paradox and Saladino’s Carnivory
Fiber or Not: Short-Chain Fatty Acids and the Microbiome
Are ‘vegetarians’ or ‘carnivores’ healthier?
Vegetarianism is an Animal-Based Diet
Being “mostly vegan” is like being “a little pregnant.”
Plant-Based Nutritional Deficiencies
True Vitamin A For Health And Happiness
Hubris of Nutritionism
Ancient Greek View on Olive Oil as Part of the Healthy Mediterranean Diet
Wild-Caught Salmon and Metabolic Health
Early Research On the Industrial Diet
Amish Paradox
Moral Panic and Physical Degeneration
Health From Generation To Generation
Dietary Risk Factors for Heart Disease and Cancer
Ancient Atherosclerosis?
Multiple Sclerosis and Carnivore Diet